How can GM-CSF be delivered to the alveoli with a nebulizer?
How do nebulizers produce mist?
Two types of nebulizers are available for GM-CSF inhalation therapy: a jet-type nebulizer and a mesh-type nebulizer. Both can generate fine particles (mist) up to about 3μ.
The biggest difference between the two is not the particle size of the mist, but the density of the mist. Mesh-type nebulizers are said to have a higher density mist. This is because the mist is created in a completely different way. (Ultrasonic-type nebulizers are not recommended as ultrasound waves may destroy the GM-CSF.)
Mechanism of Jet-type Nebulizers
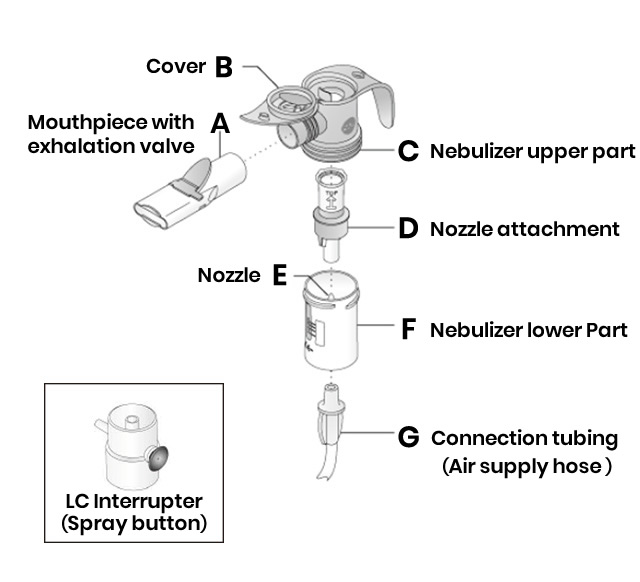
Jet-type nebulizers require a compressor (pump) to push air into the inhaler. Take the PARI LC Sprintstar nebulizer as an example.
Air is sent from the pump through the "air supply hose" shown in the figure on the left and is blown out vigorously from the small hole in the nozzle E at the bottom (F) of the nebulizer.
A cylinder called the "insert" (D) is inserted into the nozzle, and the GM-CSF solution, placed in the bottom of the nebulizer, rises to the top of the nozzle by capillary action through the gap between the nozzle and the insert. The flow of air blown out from the nozzle tends to lift up the surrounding GM-CSF solution by Bernoulli's principle. At this time, the drug solution becomes a fine mist and accumulates in the cylinder at the top of the nebulizer. When you add the mouthpiece and breathe in air, you will inhale the mist inside the cylinder.
The amount of air inhaled is thought to be about 400 to 500 mL at a time, but the rate at which mist-containing air exits the nebulizer is 89 mL per second, so the plastic valve (part B in the figure) opens to compensate for the inadequate amount of air. While diluting the accumulated mist, outside air enters and is sucked into the mouth through the mouthpiece.
Mechanism of Mesh Nebulizers

Mesh nebulizers use a specially shaped metal membrane, with thousands of holes, that vibrates at high frequencies. This vibration makes it possible to generate mist without heating the chemical. Although the protein structure of GM-CSF is very complex, it passes through the membrane only once during micronization, so it is not destroyed. Therefore, the GM-CSF in the mist remains biologically active and can be effective once it reaches the alveoli.
How can we efficiently deliver GM-CSF to the alveoli?
How does inhaled GM-CSF reach the diseased area? Figure 1 below is a schematic diagram of the human bronchus.
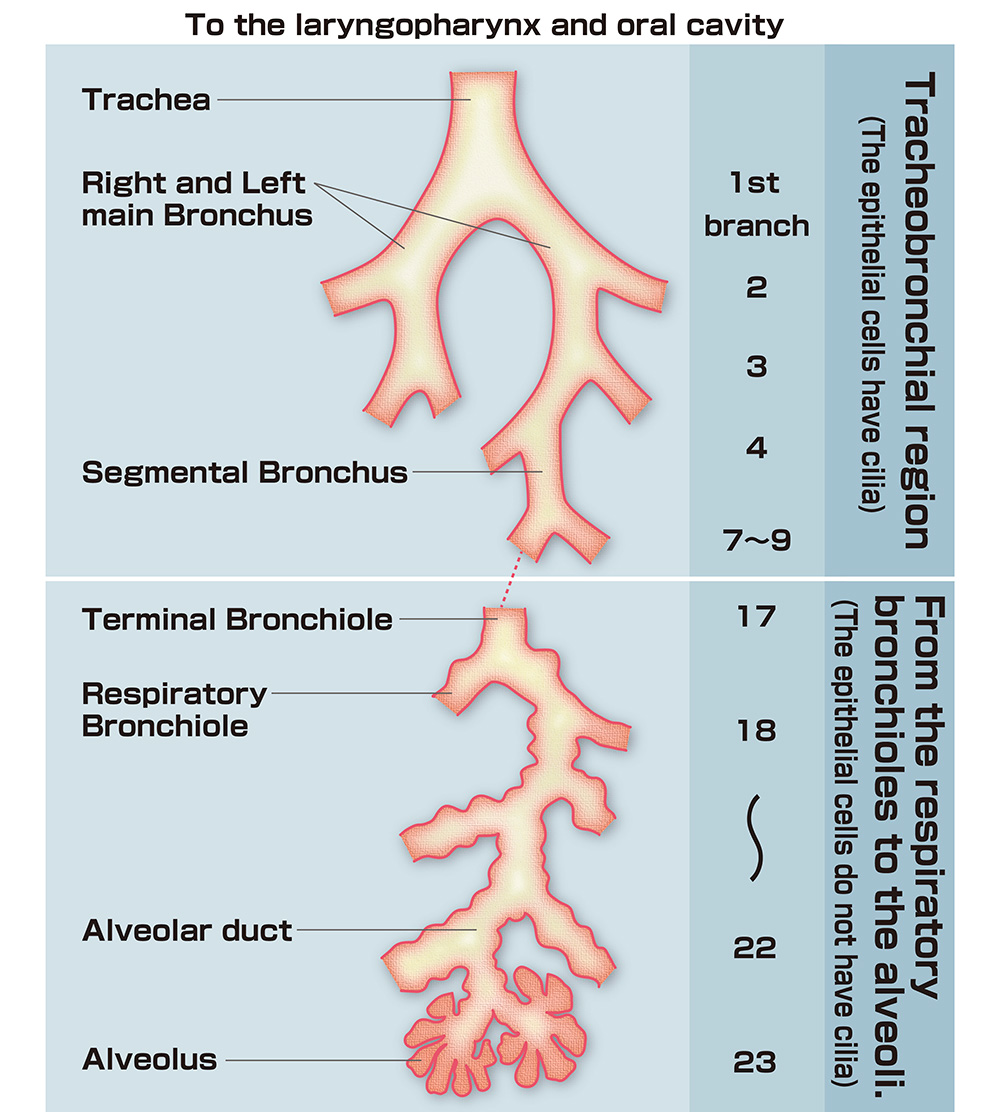
Nebulizer particles that travel far reach the alveoli
Inhaled air passes through the 12-cm-long trachea and is channeled into either the left or right main bronchus. From there, the respiratory tract continues to branch, and after branching 17 times, the terminal bronchiole is reached. In adults, the diameter of the trachea is 1.8 cm, and the diameter of the terminal bronchioles is 0.054 cm (0.54 mm). The flow velocity in the trachea when breathing air is 390 cm/sec, but when it reaches the terminal bronchioles, the air velocity decreases to 5.4 cm/sec.
The end of the terminal bronchiole is called the respiratory bronchiole, which becomes a thin tube of 0.04 to 0.05 cm, finishing at a dead end. These ends are called the alveoli. The velocity of inhaled air decreases to a very low 0.09 cm/sec before reaching the alveoli.
Patients with pulmonary alveolar proteinosis have difficulty breathing because waste materials accumulate in the alveoli, reducing the efficiency of oxygen extraction from the air into the blood.
GM-CSF inhalation therapy requires that inhaled particles (about 3 to 5 μm in size) reach the alveoli where the disease is located. Up to the terminal bronchi (17 in Figure 1), the walls of the bronchi are covered by cells with cilia, and if particles stick to the walls, the movement of the cilia causes them to be expelled upwards, turning into sputum, and passed through the mouth. It either leaves the mouth or gets swallowed and digested. By contrast, particles that reach the respiratory bronchioles and stick to their walls can spread slowly along the walls and into the alveoli.
Depending on the type of inhaler, more than 90% of the GM-CSF particles inhaled stick to the walls of the mouth, pharynx, larynx, trachea, and bronchi and are eventually expelled. Depending on the method of inhalation and the performance of the nebulizer, it may be less than a few percent. The particles reach the respiratory bronchioles (18 to 22 in Figure 1) and reach the alveoli by diffusion.
Spray button

To use the nebulizer, first attach the spray button (shown in Figure 2 below) to the bottom of the nebulizer (included with the PARI BOY Pro, which can also be purchased separately) so that the mist only comes out when you breathe in.
If you supply mist during exhalation, the particles will come out and be wasted. Using this method, particles can be inhaled efficiently.
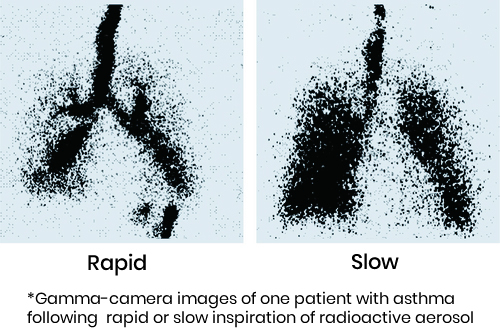
One should breathe as slowly as possible. With a rapid breathing rate, as shown on the left in Figure 3, the inhaled drug solution only reaches the terminal bronchi and does not easily reach the alveoli. When you breathe slowly, the drug solution reaches your lungs, as shown on the right in Figure 3.
Differences in inhalation effects due to differences in inhalation speed
So, how exactly can GM-CSF be inhaled to reach the alveoli efficiently? Next, the breathing method is introduced.

