What kind of treatment will the doctor provide?
Treatment of autoimmune pulmonary alveolar proteinosis
Most autoimmune pulmonary alveolar proteinosis is slowly progressive, stable, or resolves spontaneously without treatment. In rare cases, the disease progresses rapidly.Progressive cases require treatment.
The progress of the disease can be determined by measuring the oxygen partial pressure in the arterial blood, by taking blood from the artery after 5 minutes of resting and lying supine (on one’s back). The partial pressure of oxygen in a healthy person is approximately 80 to 100 mmHg (millimeter mercury).
Degree of progress of the disease according to partial oxygen pressure
| ≧70 mmHg | Mild. Even if the patients have alveolar proteinosis, there is no need for active treatment, but visit your doctor every 3 to 6 months to check whether the disease is progressing. |
|---|---|
| 60–70 mmHg | Moderate. Although the condition is not immediately dangerous, it is time to plan for treatment. The doctor will probably consider whether to administer GM-CSF inhalation therapy (described later) or lung lavage therapy. |
| 50–60 mmHg | This is a serious condition in which surfactant accumulates in the alveoli. The patient needs to get treatment. Respiratory failure means that the lungs are not able to take in oxygen properly. For outpatient treatment, please receive home oxygen therapy. Without oxygen, this condition will place a strain on the heart, increase the number of red blood cells, and make the patient more likely to develop complications. |
| ≦50 mmHg | This indicates a very seriously ill patient. Unlike other lung diseases, patients may not complain of difficulty in breathing even with this level of hypoxia. However, it is still a dangerous condition, so please seek treatment as soon as possible. |
Treatment Methods
1) Whole lung lavage
Under general anesthesia, a special bifurcated tube is inserted through the mouth into the trachea, and the tips of the tubes are placed in the right and left bronchus. When washing the right lung, the left bronchial tube is connected to a ventilator that artificially pumps air in and out to aid breathing, while the tube leading to the right bronchus is connected to a saline bottle.
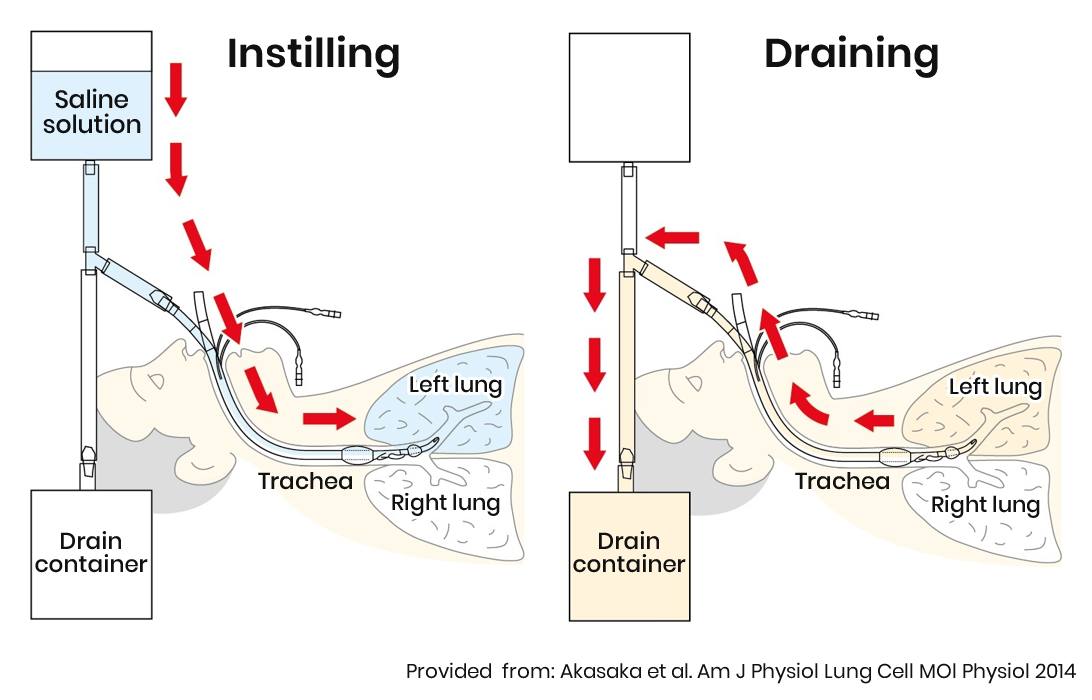
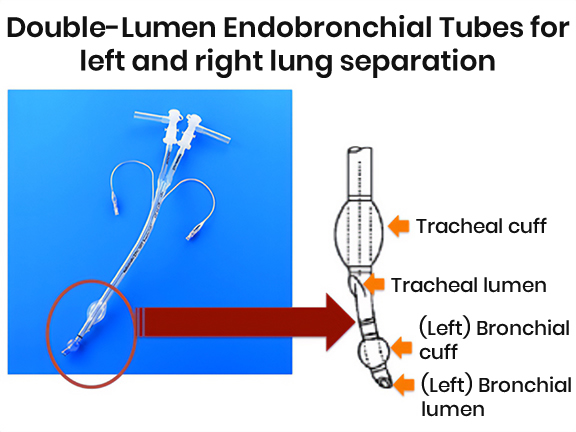
When washing the left lung, the tip of the tube is advanced into the left main bronchus, and the left bronchial cuff is inflated. Saline is repeatedly injected and collected into the left lung through the tip of the left bronchial tube. Whole lung lavage is safe because it washes only one lung at a time, allowing breathing with the unwashed lung.
For more information, please see the page "About whole lung lavage for pulmonary alveolar proteinosis."
 Whole lung lavage is being performed by Dr. Keiichi Akasaka(Saitama Red Cross Hospital)
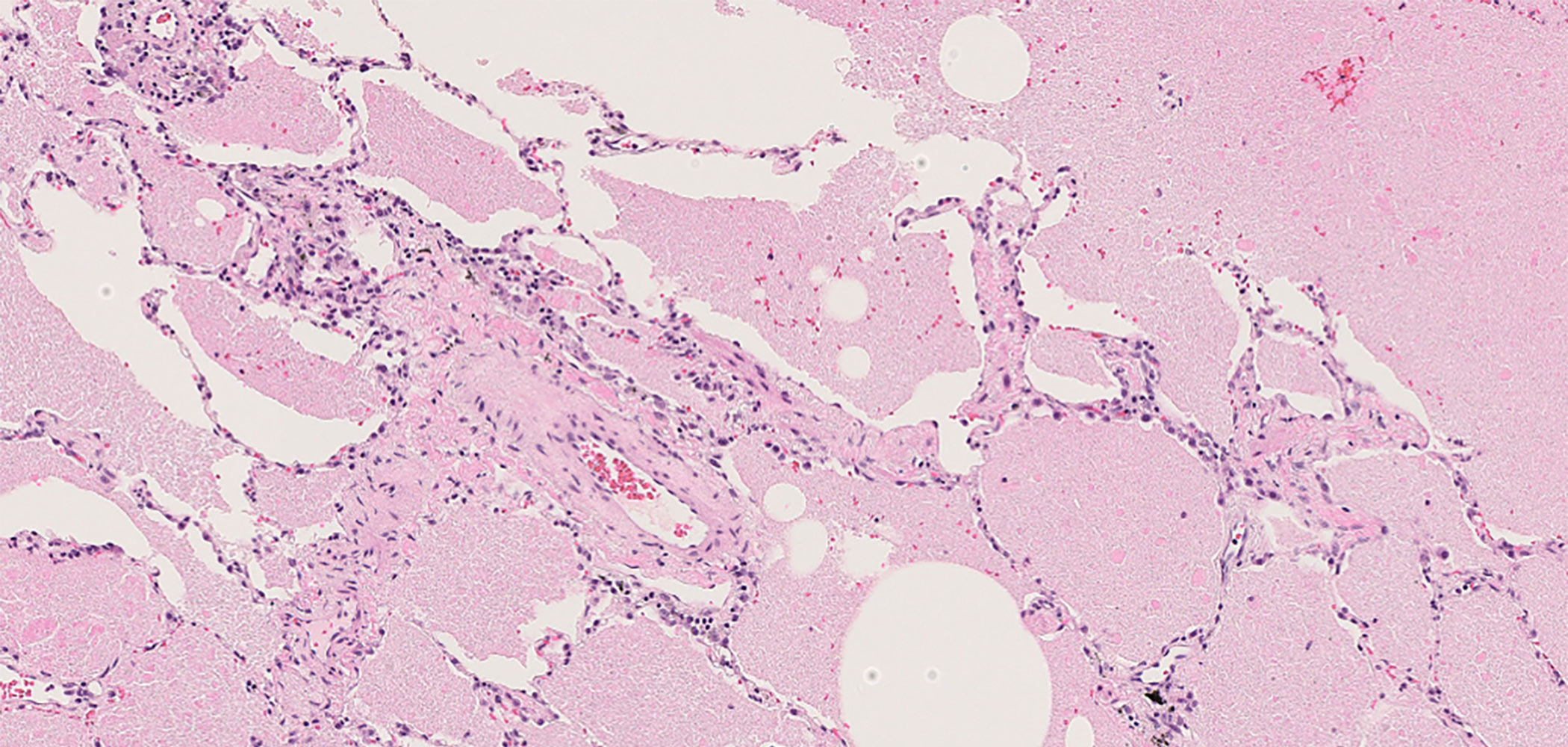
Whole lung lavage is being performed by Dr. Keiichi Akasaka(Saitama Red Cross Hospital) Bronchoalveolar lavage fluid after 20 lavages
Bronchoalveolar lavage fluid after 20 lavages2) GM-CSF inhalation therapy
(GM-CSF: trade name “Leukine” in the US, “Salgmarin” in Japan)
To undergo this therapy, dissolve GM-CSF in physiological saline and put into a nebulizer. Inhale twice daily for 15 to 20 minutes using the nebulizer (jet or membrane nebulizer). Continue this once or twice daily for 1 week, then take a week off (a week without inhalation). Repeat this cycle 12 times. This means a total of 24 weeks of treatment. In Japan, this treatment is now covered by insurance, and doctors at many hospitals can prescribe GM-CSF.
 Figure-Left:Inhaler(PARI LC Sprintstar nebulizer)
Figure-Left:Inhaler(PARI LC Sprintstar nebulizer)Figure-Right:GM-CSF inhalation therapy being performed